Primary care, ER problems highlight a health-care fix with long way to go, Chender says

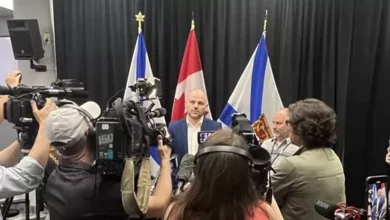
NDP Leader Claudia Chender said she left a Tuesday meeting with Health Minister Michelle Thompson with serious questions about the government’s commitment to connect Nova Scotians with primary care providers.
“This is something we focused on,” Chender said.
“There are more entry points now — virtual care and pharmacy clinics — but we also know there are still over 140,000 Nova Scotians who have identified themselves as not being attached to a family practice and that remains really concerning for us.”
Chender said that halfway into a mandate of a government that pledged to fix health care “there isn’t really a light on the horizon for a lot of folks around knowing that there is an office they can call.”
Chender said the NDP would welcome that office being a collaborative care environment and not necessarily a family doctor.
The meeting between Chender, her NDP colleague Susan Leblanc, the MLA for Dartmouth North and the party’s health critic, and Thompson came about because of a testy question period exchange on the floor of the legislature on Nov. 3.
Chender had asked Premier Tim Houston a series of pointed questions about emergency room wait times at Nova Scotia hospitals and the premier replied that all negative outcomes are problematic and painful.
“I’d be happy to walk the member through all of the various innovations that we’ve made to improve health care,” Houston said.
“I thought they’d be a receptive audience, I’d be happy to invest that time.”
Chender took the premier up on his offer but the meeting and time invested was shifted to the health minister.
“We heard a lot about the various work that the department is doing in health care, and certainly we’ve heard a lot about that in the various announcements that come out daily,” Chender said of the meeting.
“We definitely left as concerned as we were when we came in about the timeline for Nova Scotians to actually know that they are attached to primary care and we also remain concerned about the state of our emergency rooms, how many of our community hospital emergency rooms will remain open and the continuing stress on our regional hospitals.”

Chender said work is being done but “we didn’t hear a lot to suggest those situations are going to change anytime soon.”
Craig Beaton, the associate deputy minister of the provincial Health Department, told a legislative Health Committee meeting Tuesday that Nova Scotia has had a net gain of 150 new physicians from September 2021 to September 2023, including 312 new starting physicians in the province and 163 departures.
“We do know that a lot of our physicians stay when they come,” Nicole Boutilier, vice-president of medicine with Nova Scotia Health, told the committee.
“We have a 90 per cent retention rate,” she said, adding that the reasons for leaving among the 10 per cent of recruited doctors who don’t stay are most often family situations of living in a different area than family or moving on to get more training or to do specialized work.
At that committee meeting, Leblanc raised a statistic that Chender had presented to the premier in that November question period exchange, that more deaths occurred in Nova Scotia ERs in the first nine months of this year than in the entire record-breaking year of 2022.
LeBlanc wanted to know if there was a connection between ER wait times, resources and ER deaths.
“Having more resources will, I think, overall improve the environment and the care would be better for everybody, but I don’t think you can make the connection between increasing fatalities with the resource issue that we have,” Dr. Colin Audain, president of Doctors Nova Scotia said.
Boutilier said the number of patients presenting at emergency with critical issues is going up.
“Whether it’s folks going into the OR or folks going to emerg, the acuity that the doctors are experiencing is much higher than they’ve ever experienced,” Boutilier said.
“It has a lot to do with COVID . . . and also the general frailty and age of our population has made presentations that much more acute in emerg.”
Aside from the 145,000 people on the Family Practice waitlist and the escalating number of ER deaths, an NDP news release that preceded Tuesday’s health meeting pointed to more ambulance response times missing the target, a decrease in the ambulance offloads taking less than 30 minutes and the number of family physicians per capita getting worse.
The committee heard from Boutilier on Tuesday the province has developed a kind of “spoke model for a physician,” to work at one of the 10 provincial regional hospital ERs and to be able to support a community ER, as well.
Chender said that in an ideal system with regional hospitals fully staffed all the time and equipped with all the infrastructure and health-care personnel required, that type of care would work.
“We’re not in an ideal situation,” Chender said.
“We’re in a situation where over 100,000 Nova Scotians are unattached to primary care, we’re in a province with some of the highest rates of chronic disease and disability in the country and a rapidly aging population.”
Chender said the models sound good but, in the real world, “we hear from Nova Scotians all the time who just feel abandoned by the health-care system.”
Chender said there are lots of solutions needed.
“This government calls themselves solutionists, they came in promising change, and the question we’re asking is where can we see that change and so far I think that’s a real challenge for folks.”