TB advocates hail price drop of key tests but say Big Pharma could do more to stop ‘price gouging’
Every 20 seconds, someone dies of tuberculosis. But health advocates and experts are hoping that a newly announced reduction in the cost of testing for TB might change that.
On Tuesday, several TB-focused organizations announced a major victory, with multinational conglomerate Danaher reducing the cost of key tests for TB infection and resistance to a commonly used drug by 20 per cent.
This is the first time the cost of the tests has been reduced in more than 13 years, said Stijn Deborggraeve, diagnostics advisor for the Médecins Sans Frontières Access Campaign.
According to a press release on the announcement from the Global Fund to Fight AIDS, Tuberculosis and Malaria, “five million additional tests can be procured with this lower price.”
“I very much welcome Danaher’s commitment, which should enable significantly expanded access to the communities most in need,” said Peter Sands, executive director of the Global Fund, in the release.
“I’m very happy,” said John Green, a New York Times best-selling author and viral YouTuber who has garnered a reputation as a philanthropist and TB advocate — but he still sounded a cautious note.
“When good things happen, you want to celebrate,” said Green. “But at the same time, I’m conscious of the fact that 1.6 million people are going to die of TB this year.”
‘It’s human choice’
TB is the deadliest disease in human history and has killed an estimated one billion people in the last 200 years. Caused by a bacterium called M. tuberculosis, TB is curable in virtually all cases, and has been for 70 years, thanks to powerful tests, medications and treatment regimes.
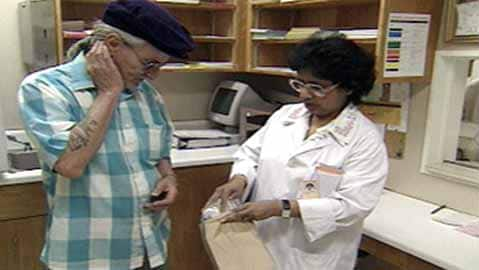
WATCH: A CBC report on tuberculosis from the 1990s:
Public health nurses visit TB patients to ensure they follow a drug regimen of eight pills daily for up to a year.
But according to experts, pharmaceutical companies are overcharging for critical treatments developed with hundreds of millions of dollars in public funding, locking out those who need them most.
The fact that 1.6 million still die of the disease every year is a testament to what happens when you put profit over patients, says Green.
“The real cause of tuberculosis in the 21st century is not a bacteria,” said Green. “It’s human-built systems. It’s human choice.”
On Friday, world leaders are set to meet in New York for the second-ever United Nations High Level Meeting on TB. Advocates and experts hope to see promises of progress, not just from governments, but corporations as well.
“We can choose a world where no one dies of TB, just as we are currently choosing a world where 1.6 million people do,” Green said.
TB is an airborne infectious disease that typically infects the lungs, but can colonize almost any part of the body. A third of all people globally are estimated to have a latent TB infection and more than 10 million get sick every year.

Despite a cure, TB has remained the world’s deadliest infectious disease nearly every year going back to the Black Death. The only exceptions in that time were 2020 and 2021, when it took second place after COVID-19 — even though the number of deaths from TB went up.
As of 2022, TB is back on top.
TB tends to strike the most vulnerable, including young children and immunocompromised individuals. People in poor living conditions or with little access to health care, such as those in impoverished countries or Canada’s Indigenous communities, are also at higher risk.
‘Printer ink’ model for life-saving tests
But diagnosing TB is a challenge. One of the only reliable methods is to use molecular tests, said Carole Mitnick, a professor of global health at Harvard Medical School and a leading expert in TB treatment.
Part of the problem, Mitnick said, is that one multinational conglomerate holds a virtual monopoly — namely, Danaher, whose subsidiary Cepheid produces the GeneXpert molecular testing system.
Since the GeneXpert system went to market in 2006, it has been sold under a “printer ink” or “razor blade” model — that is, a company sells the base of a product at relatively low cost (like a printer or a razor handle) but charges high amounts for the required disposable or single-use components (like ink cartridges or razor blades).

The testing machine, which can also be used to diagnose HIV, hepatitis, COVID-19, Ebola and a host of other diseases, is relatively affordable, Deborggraeve said. MSF gets machines that can run four tests at a time for $17,000 to $20,000 US.
Many low-income countries got them years ago, when sales were subsidized by public funding, said Mitnick.
But that locks them into the GeneXpert system and forces them to buy the company’s single-use TB test cartridges, which have been sold at a high markup for over a decade.
For all tests but one, those markups will continue.
Danaher and Cepheid did not respond to CBC’s request for comment.
Profit margins as high as 500%
Danaher is a multinational conglomerate and holding company that had profits of $7 billion US in 2022.
GeneXpert was developed using more than $250 million US in public funding, much of which came from Canadian and U.S. taxpayers. A Médecins Sans Frontières (MSF) study that investigated the public funding concluded that “the key role played by the public sector in R&D and rollout stands in contrast to the lack of public sector ability to secure affordable pricing.”
The company has long refused to disclose the cost of producing the TB test cartridges. In 2018, MSF commissioned an independent analysis that concluded each cartridge costs around $3 to $4.50 US to produce at the volume required in 2018.
In their statement this morning, Danaher claimed that at $7.97, they would be selling the basic TB cartridges at cost.

For decades, Danaher has sold them to impoverished countries and organizations delivering treatment in those communities for $10 to $15 apiece, a markup of 250 to 500 per cent. At this price point, widespread molecular testing is out of reach for many countries with the highest burdens of TB.
The experts CBC spoke with said that since the study was conducted in 2018, the number of cartridges sold has increased dramatically, meaning the cost of production is now likely even lower.
With the new pricing, Danaher now charges almost double for cartridges capable of detecting extensively drug-resistant TB (XDR-TB), despite the fact they cost the same to produce.
“It’s pure price gouging. It’s pure profiteering,” said Deborggraeve before the announcement.
With the price reduction in only one type of test, that’s still the case for most of Cepheid’s GeneXpert cartridges, Deborggraeve said in an interview Tuesday.
“We invite the companies to be transparent in the costs … so that countries don’t have to buy blindly.”




