Health officials field pointed queries on physician retention, ER closures in N.S.

Health officials made best efforts Tuesday to tout improvements in doctor retention and ER closures in Nova Scotia.
The Liberal and NDP members of the legislative health committee weren’t buying it.
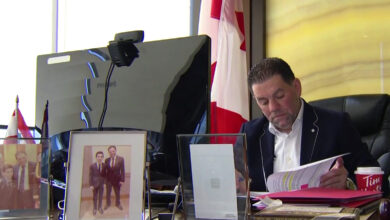
“For the last year, until the end of October, we have just over 100 physicians (recruited) and when you take all of the ins and outs, the net of that is 65 to 70 physicians,” Karen Oldfield, interim CEO of Nova Scotia Health, told reporters after the meeting.
“We’re on track to do the same as we have and perhaps to do a little bit better than last year. That’s all physicians, not just family physicians. That includes specialists as well.”
On track is good, but “never enough,” Oldfield said.
“We all know the importance of primary health care and we have to do as much as we can as communities, as a government, as a health system, as people to recruit to our province.”
The New Democratic Party was quick to point out in a news release preceding the committee meeting that more than 145,000 Nova Scotians are on the family practice wait list for a primary care provider and chronic emergency room closures continue throughout the province.
Net gain
Kelly Regan, the Liberal MLA for Bedford Basin, wanted to know how long recruited doctors are staying in the province, how many are leaving after one year and why.
“We know that over the last two years we’ve had a net gain of 150 physicians into Nova Scotia,” replied Dr. Nicole Boutilier, vice-president of medicine with Nova Scotia Health.
Craig Beaton, the associate deputy minister of the provincial Health Department, said Nova Scotia has had a net gain of 150 new physicians from September 2021 to September 2023, including 312 new starting physicians in the province and 163 departures.
“We do know that a lot of our physicians stay when they come,” Boutilier said. “We have a 90 per cent retention rate. With the 10 per cent that have left, we do exit interviews on people who aren’t retiring and the majority of the reasons that they are leaving are for family reasons, they live (here but have) family in other parts of the country, or they leave to get more training and to do specialized work that they may or may not bring back to Nova Scotia.”
Regan said many physicians change how they are practising and even though they are still listed as a doctor, they provide a reduced level of service.
The effect of those reductions has not been measured, she was told.
Susan Leblanc, the New Democratic MLA for Dartmouth North, wanted to know how many ER physician vacancies exist in the province and asked about the increase in ER deaths, with more deaths occurring in Nova Scotia ERs in the first nine months of this year than in any of the entire last five years.
Jeannine Lagasse, deputy minister of the Health Department, said the ER physician vacancies answer was not available.
Leblanc asked about connections between wait times to see a doctor, a general deficiency of health care among Nova Scotians and the increased ER deaths.
Dr. Colin Audain, president of Doctors Nova Scotia, said emergency departments triage the most urgent patients and they would not be the ones waiting.
“Having more resources will I think overall improve the environment and the care would be better for everybody, but I don’t think you can make the connection between increasing fatalities with the resource issue that we have,” Audain said.
Critical patients
Boutilier said the number of patients presenting at emergency with critical issues is going up.
“Whether it’s folks going into the OR or folks going to emerg, the acuity that the doctors are experiencing is much higher than they’ve ever experienced,” Boutilier said. “It has a lot to do with COVID … and also the general frailty and age of our population has made presentations that much more acute in emerg.”
Regan referenced statistics for unplanned ER closures between April 2021 and March 2022 accounted for 31,697 hours or 1,320 days, double from the previous year.

“This puts further strain on other, open ERs like Cape Breton Regional Hospital or the hospital in Kentville,” Regan said.
The Bedford Basin MLA asked if any of the witnesses had the numbers for unplanned closures over the past year but Lagasse said those figures were still being finalized.
Regan asked when the ER at Soldiers Memorial Hospital would be reopened or if the plan was to permanently shut it down.
“There is no intention to permanently shut down the emergency at Soldiers,” Oldfield replied. “In fact, that is one of the places I visited just three weeks ago and I can assure you there is every intention to recruit and to augment the hours.”
Oldfield said a new physician will start in January and split time between Valley Regional Hospital in Kentville and Soldiers.
Baddeck hospital
Oldfield said the Victoria County Memorial Hospital in Baddeck has a very complicated emergency department, one that is very important to the entirety of Cape Breton Island.
“They would love to get back to an ER, we have urgent treatment there,” Oldfield said.
One of the challenges with Baddeck is that when the ER was operating, many people were coming from over the mountain, from the Sydney area, and consequently the ER was overwhelmed, she said.
“One of the beauties of the emergency system all working together is our 10 regional centres (regional hospitals) as well as our tertiary centre never close,” Boutilier said.
“We’re quite unique in the country with that in that we have not had an (ER) closure in those types of facilities.”
Boutilier said the system often draws resources from outside the regional centres to keep the system stable.
“It does depend from month to month what the hours will be,” at the smaller facilities.
“We have developed a way of having kind of a spoke model for a physician, where they can be committed to a site but have a bonus to be able to support a community site as well. As we hire more people and they come into that new system, we’re hoping that’s going to beef up that support to those Level 3 emergency rooms.”