More stories of long ambulance wait times in Nova Scotia signal that health care getting worse, not better – Churchill

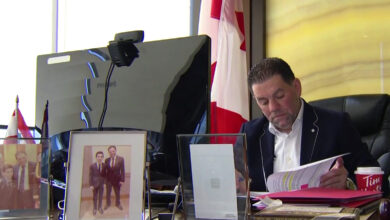
Nova Scotia Liberal leader Zach Churchill says three incidents of long ambulance delays in the Annapolis Valley over the past few months highlight that the Nova Scotia health care system is getting worse, not better.
“There does seem to be a real disconnect between what the government is saying on how good everything is in health care and the stories we’re hearing from patients and doctors and other health care workers in the system,” Churchill said.
“These long wait times to get an ambulance are another example of the situation not improving but getting worse in health care.”
He said offload wait times have been getting worse, with ambulances taking longer to discharge patients in emergency departments.
“We’ve heard of patients waiting for more than 10 hours to go from the ambulance to the emergency room, which is holding up the fleet of ambulances from getting out to other emergencies.”
The regular closure of rural emergency rooms is also playing a factor, especially when ERs at the hospitals in Middleton and Digby are happening at the same time, Churchill said. That leaves the closest emergency rooms in Kentville and Yarmouth, creating long travel times that can tie up ambulances even before they wait to offload.
“It creates a big gap in emergency services in the Digby-Annapolis County areas. (That’s) a big stretch of land with fewer options to get to emergency rooms,” he said.
“We’re certainly seeing disturbing stats and hearing about really scary stories.”
He said paramedic, nurse and other critical position staffing levels are also part of the problem, and “I think the working conditions are really affecting the recruitment and retention of people into the health-care system because a lot of people know how bad it is in there.”
On Sept. 7, a high school soccer player who was slipping in and out of consciousness after an episode during a practice in Canning waited 45-50 minutes for an ambulance because the closest was in Halifax County.
A person at the practice, who asked not to be named, said there were many attempts to call for an update while coaches and players waited. They called it a “scary event” as the girl alternated between being responsive and non-responsive.
Four days earlier, it took an hour for the first ambulance to arrive at the scene of a single-vehicle crash on Central Avenue in Greenwood. A car left the road at 9:15 p.m., hit a tree stump and flipped, tearing the motor from the vehicle.
RCMP spokesman Cpl. Chris Marshall said a 30-year-old man had to be airlifted to hospital from nearby 14 Wing Greenwood, after that first ambulance arrived. A 37-year-old man who was a passenger had to wait for close to two hours before the second ambulance arrived on the scene to transport him to hospital.
One of the car’s occupants could be seen from a nearby parking lot, laying on a backboard on the curbside behind a firetruck waiting for an ambulance, witnesses said.
On July 24, in Wolfville, a man from Ontario laid on the street for about hour and a half with a broken leg waiting for an ambulance after losing his balance and falling under his motorcycle while trying to manoeuvre it in a parking spot.
Marshall said a passing RCMP member was waved down by a member of the public and remained on scene until the ambulance arrived. He said the officer arrived at 5:15 p.m. and left the scene at 6:50 p.m.
In an emailed statement, the Department of Health and Wellness said it takes its responsibility for patient care seriously, and the last thing it wants is for residents of the province to experience long waits.
“We recognize that in some cases, there are factors that may contribute to longer wait times, but we do everything possible to avoid that from happening,” the statement said.
It said that care starts when 911 is dialed, not just when the ambulance arrives.
“For example, we added a nurse to the EHS medical communications centre, that works alongside a physician and paramedic specialist to assess each caller virtually once it’s determined that the emergency is not life-threatening.”
The department also said it has done other things to address delays, including increasing single paramedic response units that can treat and discharge patients on the scene, and adding a new LifeFlight plane to transport non-critical care patients from Sydney and Yarmouth to Halifax. That has happened 92 times, which the department said equals about 920 more hours that ambulances have stayed in their community.
Also in an email, a spokeswoman for Emergency Medical Care, which provides ambulance service in the province, said the number of ambulances available varies day-to-day based on the needs.
“Similarly, the average number of ambulances that are not staffed is a difficult number to calculate given the variety of vehicles employed to manage system capacity and the real time impact of ambulance offload delay,” Brittany Mitchelmore said. “These capabilities include emergency ambulances, patient transfer vehicles, and support units staffed with a variety of care providers to ensure the most appropriate care at the right time.”
She said the review of daily, weekly, monthly, quarterly, annual and time-dependent reports “monitor the performance of the EHS system and provide insight into demands and trends, which allow appropriate resource changes and additions to be made within the system in order to provide the right resource to the right person at the right time for the right reason.”
Paramedicine is faced with the same recruitment challenges as other health care professions, Mitchelmore said.
“Recruitment efforts are focused on local recruitment and also international recruitment. EMC’s key focus remains on what we can do to improve our employee experience for our teams and also how we can attract and retain new paramedics.”
On Tuesday, the province’ auditor general, Kim Adair, will release her performance audit on ground ambulance services. The report examines whether ground ambulance services are meeting the needs of Nova Scotians in a cost-effective manner.